I often get asked - can I get dental implants if I have osteoporosis? The good news is that, generally, the answer is yes, you can get dental implants despite having osteoporosis. The bad news is, it needs special finessing, expertise, and healing time to be successful. Let's delve more deeply into the topic.
What Is Osteoporosis?
The word “osteoporosis” means “porous bone.” The disease happens when the density and quality of a person’s bones lessen, usually as we age. To understand osteoporosis, you first have to understand how bones behave in the body. Think about your skin. Old cells are sloughed off and new cells are constantly being created that are more supple than the old ones. The same type of behavior happens in bones. At any given time, some of your bone cells are creating new bone (osteoblast) while other bone cells are breaking down older bone (osteoclast). In other words, one type of bone cell makes and the other type of bone cell takes away. The process of replacing old bone with new is called remodeling. The entire human skeleton regenerates over about 10 years.
When we’re younger, more of the cells are creating new bone, building bone strength and density. But as we age, the balance shifts. Osteoporosis happens when more bones are breaking down than are being created. In people with osteoporosis, the bone is softer and more brittle.
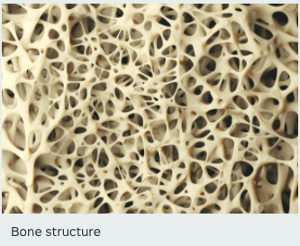
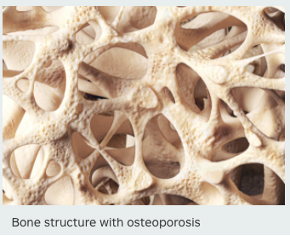
That’s because bones are structured like honeycombs. With osteoporosis, the holes in the honeycombs get bigger, making them less dense and more susceptible to cracks and breaks. That leads to fractures, most often of the hip, spine or wrist.
Quick Facts
|
Osteoporosis happens to the jawbone just like it does to any other bone. This loss of bone density in the jaw makes the bone softer, which can lead to problems with tooth stability and can increase the risk of tooth loss, receding gums and periodontal disease. This also impacts the success of dental implants since implants need to integrate into strong bones to be stable and secure.
Techniques for Placing Dental Implants in Patients with Osteoporosis
There are a number of techniques that enable dentists to secure dental implants in patients with osteoporosis. Usually, I consider four different techniques:
Bone compression
To compress bones, instead of drilling a hole to insert the implant, the implant is pressed directly into the bone. The pressure used helps compress the bone more tightly around the implant screw so that the bone is denser and the implant is more stable.
Bone densifying
Special drills can be used to insert the implant into the bone that compacts the bone and make it denser. A thicker bone improves secure implant strength and security.
Connecting teeth
If two or three adjacent teeth are missing, instead of placing an individual implant for each tooth, connecting the teeth together as one implant distributes the bite force evenly across all three. By splinting the three teeth together, we can achieve nine times the strength of one tooth alone. This increases the likelihood that the implant will remain strong and stable over time.
Specialized implants for the upper jaw
When the teeth need replacing in the upper jaw, it can make sense to use the cheekbone (zygomatic bone) or base of the nose, or bone near the upper wisdom teeth areas (pterygoid bone). This technique is applied if the bone is really soft and/or the sinuses are enlarged.
A Word of Caution
Some patients with osteoporosis may be prescribed medicine to build up bone density called bisphosphonates, such as Fosamax® and Boniva®. In rare cases, long-term use of these medications can cause osteonecrosis of the jaw, which can lead to failure of the jaw to heal, exposure of the jaw, or even jaw bone death. That’s one reason why it is important for osteoporosis patients to tell their dentist about their condition and the medications they take so that jaw bone failure can be avoided.
Get the Expertise You Need for Dental Implants
So the answer to the question is that dental implants are an option for people with osteoporosis, but it requires special capabilities. Remember, for dental implants to be successful, you need strong bone to attach the implant. Without strong bones, it will likely take longer for the implant to integrate into the bone, which means a longer healing time before the final crowns can be placed. All these variables in treatment make it important that you find a dental implant expert with experience doing dental implants for people with osteoporosis, particularly for a full arch or full mouth replacement. An experienced dentist can make a complete evaluation of your situation and recommend a dental implant strategy to counteract your osteoporosis and lead to dental implant success.
Dr. Ramsey Amin, DDS maintains an implant only practice in Burbank, California. He performs all "full-scope implantology" with prosthetic reconstructions, including zygomatic and pterygoid implants. He is Vice President of the AAID Western District. He can be reached at https://www.burbankdentalimplants.com.